- Blog
In-Network vs. Out-of-Network
Posted on 03-02-2026 in Insurance & Price Transparency by Dr. Erik Nilssen

Posted on 03-02-2026 in Insurance & Price Transparency by Dr. Erik Nilssen
In-Network Vs Out-of-Network Providers
In-network providers have previously signed a contract that limits the amount of money (contracted rate) a provider may charge individuals who are covered under the contracted insurance company. The agreed-upon contract rate includes both the patient and insurer’s shares. The portion of the contracted rate a patient pays is determined by his or her policy.
Out-of-network providers are providers who have not agreed to accept a contracted rate with a patient’s insurance company. If a patient chooses to seek treatment outside of his or her network, insurance companies typically require the patient to pay a larger deductible, copayment and coinsurance amount.
Choosing an Out-of-Network Provider Can be Beneficial
Although seeking treatment from a provider that is not within the patient’s network is typically more expensive, there are reasons that some patients choose to seek care from providers who do not have a contracted rate with their insurance company.
An individual may choose to go out-of-network to receive treatment:
Out-of-Network Emergency Care Regulations
Due to the Affordable Care Act (ACA), all insurance plans that were sold after March 23, 2010, are required to cover out-of-network emergency care. According to the ACA, insurance companies who offer these plans cannot charge higher coinsurance or copayments if an individual receives emergency care from an out-of-network provider. Furthermore, individuals are not required to receive prior approval to receive this emergency care. However, non-emergency care must be delivered by an in-network provider and prior approval from the insurance company may be required.
It is important to note that an insurance plan purchased prior to March 23, 2010, a short-term plan and other types of coverage may not be required to follow these rules.
Patients Need to Comparison Shop
As health care costs continue to rise, patients need to shop around to find the best care at the most reasonable prices. Even individuals who plan to stay in-network should compare the prices charged by the physicians and facilities offering contracted rates.
Consider that an insurance company may pay from $500 to $3,000 for a magnetic resonance imaging (MRI) scan of the ankle and foot. If a patient who is required to pay a 20 percent co-pay for services receives an MRI at a contracted facility that charges $500, he or she will be responsible for $100; whereas, a $3,000 MRI at a different in-network facility would cost the patient $600.
Some Patients in Pensacola, Florida, Are Choosing to Pay Cash for Services
As deductibles continue to increase, some individuals are choosing to pay cash for services: Especially when they want to seek treatment from a skilled surgeon or specialist who is not contracted with their network.
For example, if a patient’s in-network deductible is $5,000 and his or her out-of-network surgical procedure costs $5,000, the patient may choose to have his or her ankle and foot surgery performed by a highly skilled out-of-network surgeon as opposed to by an in-network surgeon who does not offer the same experience and skill.
Patients should keep in mind that when they do not use their health insurance for a medical service, the money paid out of pocket to the provider will not be applied towards their deductible; however, a portion of these charges may qualify to be taken as a deduction on his or her annual income taxes.
The Future of Health Insurance
In 2016, average deductibles across the gold, silver and bronze plans of the Affordable Care Act’s exchanges increased by 8.4 percent ($265). It is projected that costs related to health insurance and health care services will continue to rise.
The 2016 Presidential Candidates, Hillary Clinton (D) and Donald Trump (R), have both stated that should they take office; changes will be made to ObamaCare. Consequently, determining the future of health care costs and health insurance is challenging. Therefore, individuals need to be vigilant in comparing the health care costs and benefits of both in-network, and out-of-network providers.
We encourage our patients to ask questions and compare prices. An injury to the ankle and foot that is left untreated can lead to a lifetime of chronic pain. For this reason, individuals should seek treatment with an experienced orthopedic surgeon.
Sources:
If you’ve ever sprained your ankle and thought, “this isn’t a big deal…it’s a minor injury,” you’re not alone. Ankle sprains are among the most common musculoskeletal injuries, especially in active adults and athletes. However, for some patients, what begins as a simple sprain becomes a frustrating cycle in which the ankle feels weak, unstable, and prone to “rolling” again and again. Understanding why this happens is the first step toward breaking the cycle and restoring long-term stability.

February is American Heart Month, a time to raise awareness about cardiovascular health and its far-reaching effects. While most people recognize the importance of heart health for longevity and disease prevention, fewer realize its critical role in musculoskeletal well-being. At North Florida Bone & Joint Specialists, we emphasize a comprehensive approach to orthopaedic care, recognizing that a strong heart supports strong bones and joints.
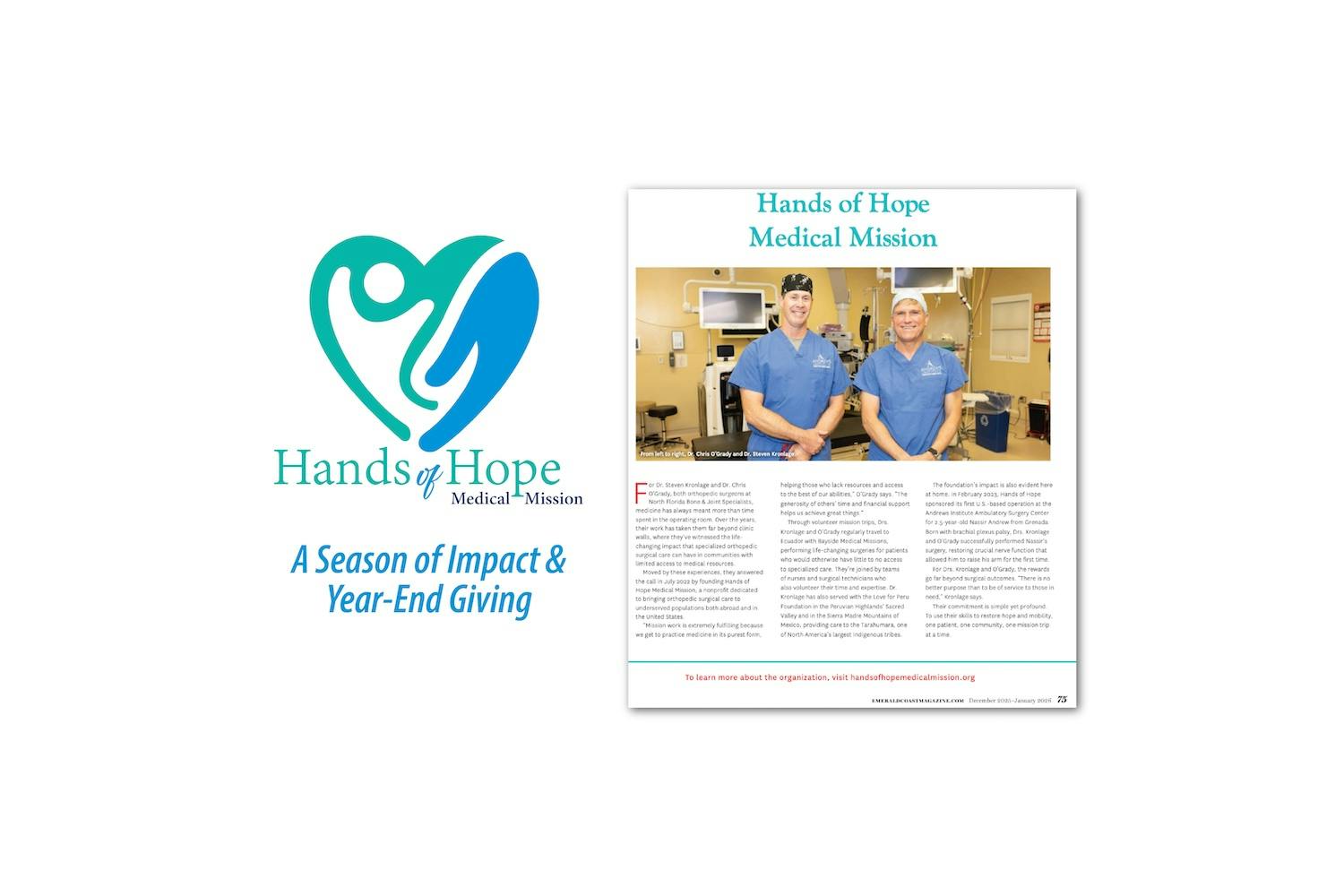
North Florida Bone & Joint Specialists is honored to share the Hands of Hope Medical Mission feature in the newly released December 2025/January 2026 issue of Emerald Coast Magazine. As part of the Medical Profiles section of this edition, the article highlights how two of our own, Dr. Steven Kronlage and Dr. Chris O'Grady, volunteer their time and talents to bring compassionate orthopaedic care to communities with limited access to medical services.