- Blog
Rotator Cuff Injuries & Treatment
Posted on 03-02-2026 in Minimally Invasive Surgery, Regenerative Medicine & Rotator Cuff by Dr. Joshua Hackel
Posted on 03-02-2026 in Minimally Invasive Surgery, Regenerative Medicine & Rotator Cuff by Dr. Joshua Hackel
The American Medical Society for Sports Medicine defines rotator cuff tears as partial or full tears of one or a number of the four muscles that help move the shoulder and keep the end of the long bone of the arm within the shallow socket of the shoulder (the “rotator cuff”). Rotator cuff tears are more common in your dominant arm. The most common symptoms of a rotator cuff tear include:
Causes of Rotator Cuff Tears
There are two main causes of rotator cuff tears – acute injury and degeneration. Acute tears can occur when you fall down on your outstretched arm or lift something too heavy with a jerking motion. This type of tear can happen with other shoulder injuries, such as a broken collarbone or dislocated shoulder. Degenerative or chronic tears are typically the result of a wearing down of the tendon that occurs slowly over time, which naturally occurs as we age. If you have a degenerative tear in one shoulder, there is a greater likelihood of a rotator cuff tear in the opposite shoulder — even if you have no pain in that shoulder. Several factors contribute to degenerative rotator cuff tears, including repetitive stress, lack of blood supply and bone spurs.
Repeating the same shoulder motions, again and again, can stress your rotator cuff muscles and tendons. Repetitive movements while playing sports like baseball, tennis, rowing and weightlifting are examples of sports activities that can put you at risk for overuse tears. Many jobs and routine chores can also cause overuse tears. The blood supply in our rotator cuff tendons lessens with age and impairs our body’s natural ability to repair tendon damage, which can ultimately lead to a tendon tear. As we age, bone spurs (bone overgrowth) can also develop on the underside of the acromion bone. When we lift our arms, the spurs rub on the rotator cuff tendon that, over time, will weaken the tendon and make it more likely to tear.
Types of Rotator Cuff Tears
Rotator cuff tears are segmented into two types, partial and full-thickness tears. Partial tears are also referred to as incomplete tears. They damage the tendon but do not completely sever it. In contrast, full-thickness tears are considered complete tears because they separate all the tendon from the bone. Essentially with a full-thickness tear, there is basically a hole in the tendon. Tears that happen suddenly, such as from a fall, usually cause intense pain. There may be a snapping sensation and immediate weakness in your upper arm.
However, tears that develop slowly due to overuse can also cause significant pain and arm weakness. You may experience pain in the shoulder when you lift your arm or feel pain that moves down your arm. This pain may be mild and only present when lifting your arm over your head at first and be relieved by taking an over-the-counter (OTC) medication, such as aspirin or ibuprofen. Over time, the pain may become more noticeable when you lie on your side to sleep. The pain and weakness in the shoulder may make routine activities such as combing your hair or reaching behind your back more difficult. Eventually, OTC medication may stop providing pain relief. It is also essential for patients to understand that having a rotator cuff tear that is not painful can be common. These tears, however, may still result in arm weakness and other symptoms.
Diagnosis & Treatment of Rotator Cuff Tears
Rotator cuff tears are initially suspected based upon clinical examination by a trained physician, with findings such as painful or limited motion in partial tears or weakness and muscle atrophy (shrinking) in complete tears. We use diagnostic studies such as MRI (magnetic resonance imaging) and innovative diagnostic options such as musculoskeletal ultrasound to visualize the soft tissues around the shoulder, including the rotator cuff, and confirm the diagnosis.
Early diagnosis and treatment of a rotator cuff tear may prevent your symptoms from worsening, get you back into your everyday routine much quicker and help improve overall treatment results. If you have a rotator cuff tear and keep using it despite increasing pain, you may cause further damage as a rotator cuff tear can get larger over time.
There are several treatment options for a rotator cuff tear, and the best option is different for every person. Dr. Hackel offers various nonsurgical treatment options, including a plan for activity modification or physical therapy to restore movement, strengthen your shoulder, improve flexibility and range of motion to support your shoulder, and relieve pain and prevent further injury. If rest, medications, and physical therapy do not relieve your pain, we also offer innovative therapeutic procedures such as Stem Cell Injections and Platelet-Rich Plasma (PRP) Therapy that provide a non-invasive approach to healing.
In partnership with the Andrews Research & Education Foundation, Dr. Hackel is also currently serving as the Principal Investigator on a clinical study using regenerative cells for patients with partial-thickness rotator cuff tears. The study uses regenerative cells from your fat tissue that are isolated, concentrated and injected into your tendon tear. The trial will evaluate the safety and effectiveness of using these cells to treat injuries compared to a steroid injection. Visit our Partial Thickness Rotator Cuff Tear Study blog post to learn more about the process, eligibility, benefits and risks of participating in the study.
Dr. Hackel is dedicated to providing his patients with state-of-the-art procedures to address their pain and help them heal. If you have sustained an injury or are suffering from chronic pain due to a rotator cuff injury or are interested in learning more about participating in the clinical study, contact our office at 850.916.8783 or use our convenient online appointment form to schedule an initial consultation with our office.
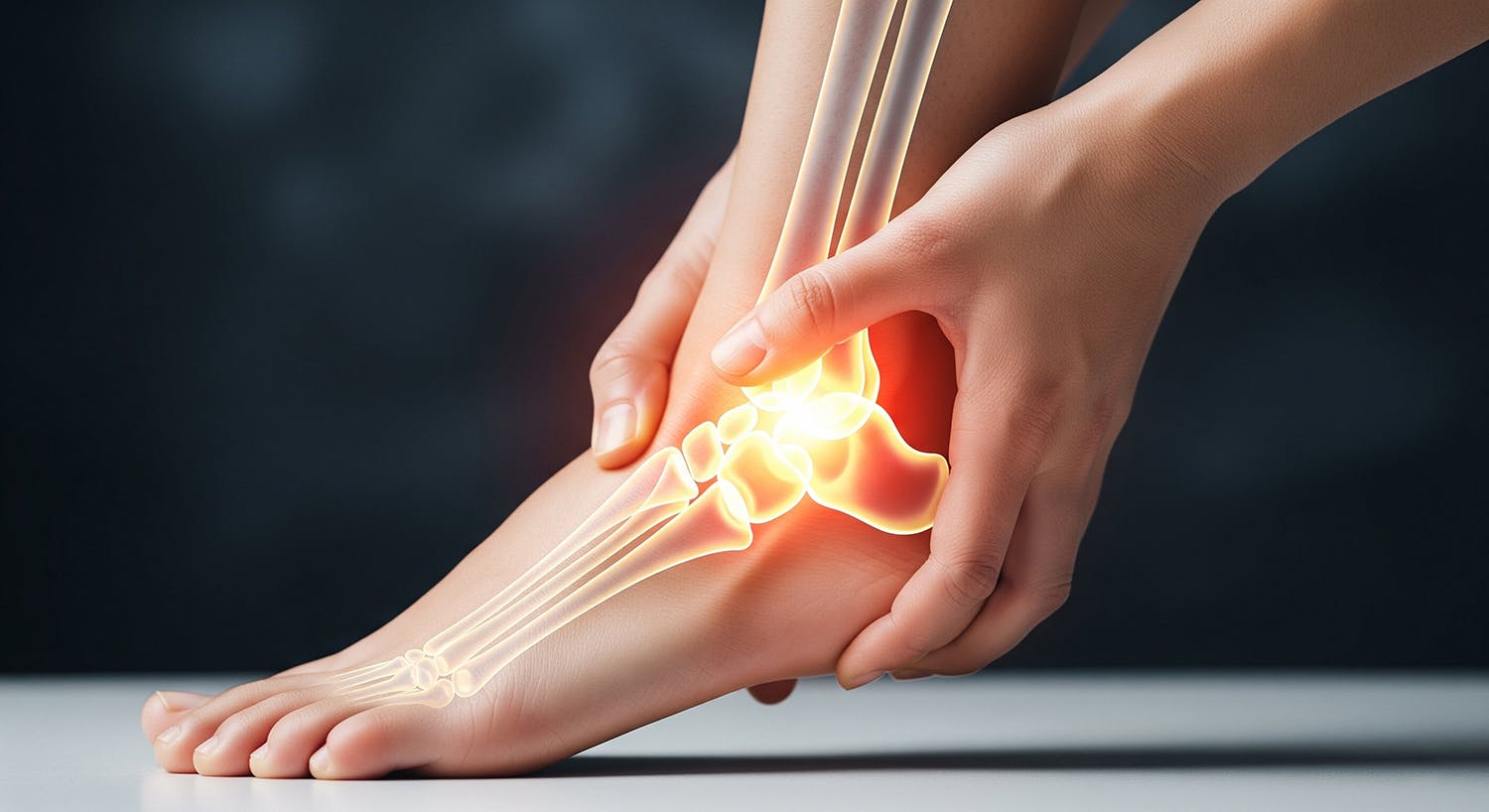
If you’ve ever sprained your ankle and thought, “this isn’t a big deal…it’s a minor injury,” you’re not alone. Ankle sprains are among the most common musculoskeletal injuries, especially in active adults and athletes. However, for some patients, what begins as a simple sprain becomes a frustrating cycle in which the ankle feels weak, unstable, and prone to “rolling” again and again. Understanding why this happens is the first step toward breaking the cycle and restoring long-term stability.

February is American Heart Month, a time to raise awareness about cardiovascular health and its far-reaching effects. While most people recognize the importance of heart health for longevity and disease prevention, fewer realize its critical role in musculoskeletal well-being. At North Florida Bone & Joint Specialists, we emphasize a comprehensive approach to orthopaedic care, recognizing that a strong heart supports strong bones and joints.
North Florida Bone & Joint Specialists is honored to share the Hands of Hope Medical Mission feature in the newly released December 2025/January 2026 issue of Emerald Coast Magazine. As part of the Medical Profiles section of this edition, the article highlights how two of our own, Dr. Steven Kronlage and Dr. Chris O'Grady, volunteer their time and talents to bring compassionate orthopaedic care to communities with limited access to medical services.