- Blog
Treating Dupuytren’s Contracture
Posted on 03-02-2026 in Hand by Dr. Alex Coleman

Posted on 03-02-2026 in Hand by Dr. Alex Coleman
Dupuytren’s Contracture can vary in severity with each case, and is initially discovered by tension in the hand, or noticing more defined ridges forming in the palm. Although there is a transformation taking place with the tissues of the hand, this disorder can be subtle and painless unless the affected area is being stretched or flattened. Seemingly simple tasks such as washing hands, putting hands in pockets or holding large objects can become difficult. Below we discuss several changes or abnormalities that may be symptomatic of Dupuytren’s, the goal of treatment and post-diagnosis care.
How is it diagnosed?
When diagnosing Dupuytren’s Contracture, your physician will risk factors such as gender, heredity, age, alcohol use and other pre-existing health conditions. Signs and symptoms include the following:
What are the different treatment options?
Although Dupuytren’s Contracture is incurable, the goal for different treatment options is to improve the overall motion and functionality of the hand. There are non-surgical and surgical treatment options available to help slow the progression of the disease and improve movement in the affected fingers. Your physician can discuss the most appropriate method based on the pathology in your hand, along with realistic goals and possible risks to manage both short- and long-term expectations.
NON-SURGICAL TREATMENT OPTIONS
Needle Fasciotomy: This procedure is also considered outpatient yet only uses a numbing injection versus anesthesia. Once the hand and fingers are numb, your physician will make a series of injections along the affected area. Slow stretches to the hand, and fingers can break the cord, allowing the hand to be straight again. This procedure can cause small tears in the skin that take a couple of weeks to heal; however, overall motion and functionality can return within a few days. The hand can be used as much as the patient is comfortable. This procedure does not remove the cord entirely from below the skin, and roughly one-third of patients will see the cord eventually return after this procedure.
Steroid Injections: Corticosteroids are powerful anti-inflammatory medications that can be injected into a painful nodule, which may slow the progression of a contracture. However, the effectiveness of a steroid injection varies from patient to patient.
SURGICAL TREATMENT OPTIONS
Fasciotomy: In this procedure, the incision is made in the palm, and then the thickened cord(s) of tissue is divided. The cord itself is not removed; dividing it helps decrease the contracture and increase the movement of the affected finger. This procedure is much less invasive and involves a local anesthetic that numbs the area without putting the patient to sleep. The wound is left open to heal gradually. Healing can vary depending on the affected area, and a splint is worn during the recovery process.
Subtotal Palmar Fasciectomy: This procedure is the more extensive of the two and often uses a “zig-zag” incision made along the natural creases in the hand where your physician will remove as many abnormal tissues and cords as possible. The wound may be left open to close on its own, or a graft of healthy skin from another area of your body may be used to close it. More healing time is involved after this procedure and can result in extensive physical therapy during recovery, along with wearing a splint.
What happens after treatment?
As with any procedure, there are associated risks and the likelihood of complications increases based on the severity of the contracture, the number of contractures addressed in a single procedure and the presence of any other medical conditions.
Post-operative care involves the fabrication of an orthosis by one of our Certified Hand Therapists to keep the fingers extended. They also provide physical therapy, including home exercise programs, that improve active range of motion and scar management and strengthening programs to regain functional use of the hand.
From consultation through to state-of-the-art post-op care with our Certified Hand Therapists at our Pensacola location, North Florida Bone & Joint Specialists is ready to support you along the way to a better quality of life. If you have noticed changes in your hands or have other concerns impacting your upper extremities, you may benefit from a consult with one of our fellowship-trained physicians. Dr. Steven Kronlage, Dr. Alex Coleman and Dr. James Piorkowski provide non-surgical treatment options and surgical intervention. Schedule same-day and next-day appointments in our Gulf Breeze and Pensacola locations by calling our office at 850-807-4200 or completing our online Appointment Request form.
If you’ve ever sprained your ankle and thought, “this isn’t a big deal…it’s a minor injury,” you’re not alone. Ankle sprains are among the most common musculoskeletal injuries, especially in active adults and athletes. However, for some patients, what begins as a simple sprain becomes a frustrating cycle in which the ankle feels weak, unstable, and prone to “rolling” again and again. Understanding why this happens is the first step toward breaking the cycle and restoring long-term stability.

February is American Heart Month, a time to raise awareness about cardiovascular health and its far-reaching effects. While most people recognize the importance of heart health for longevity and disease prevention, fewer realize its critical role in musculoskeletal well-being. At North Florida Bone & Joint Specialists, we emphasize a comprehensive approach to orthopaedic care, recognizing that a strong heart supports strong bones and joints.
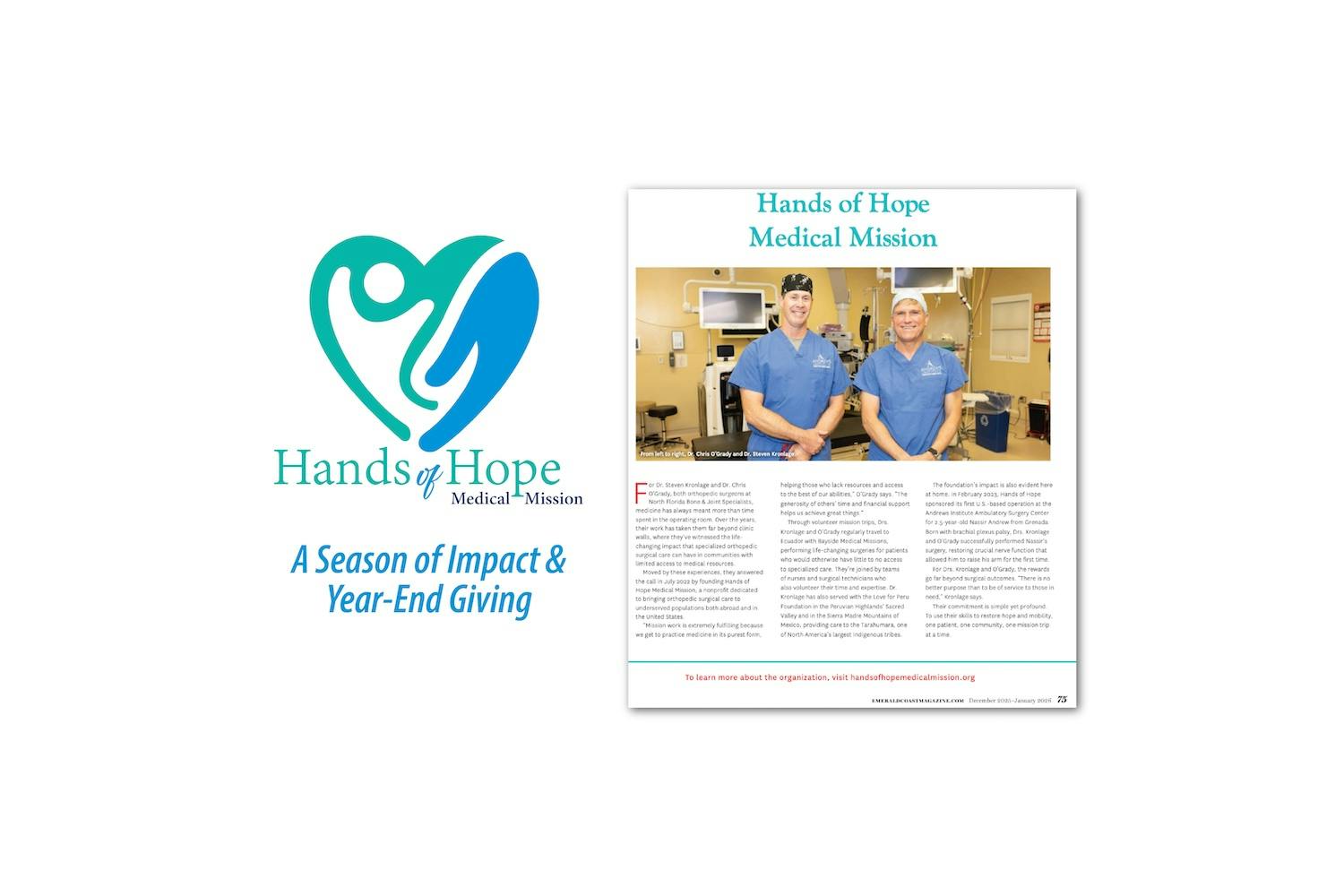
North Florida Bone & Joint Specialists is honored to share the Hands of Hope Medical Mission feature in the newly released December 2025/January 2026 issue of Emerald Coast Magazine. As part of the Medical Profiles section of this edition, the article highlights how two of our own, Dr. Steven Kronlage and Dr. Chris O'Grady, volunteer their time and talents to bring compassionate orthopaedic care to communities with limited access to medical services.